Treatment Note Resources
It is a legal requirement of our industry that Clinical Treatment Notes (including a Treatment Plan) are completed for every consultation. As a result, non-completion or partially completed SOAP notes that do not contain a Treatment Plan will not be accepted at NMK. In addition, contracted Therapists are unable to invoice for treatments where SOAP notes have not been completed in accordance with the below requirements.
** As per the relevant terms within each Team Member’s Contractors Agreement (Clause 15) or Employment Agreement (Schedule 3.1 Clause 12), all clinical treatment notes for NMK Clients:
-
must be completed at the time of the treatment/consultation, or as soon as possible afterwards; (At NMK we allow a maximum post treatment timeframe of 48hours (ie – 2days) for completion of clinical treatment notes).
-
must be completed in English, be comprehensive, accurate and completed to a legible, easily understood, professional standard;
-
must display written evidence that verbal approval for the treatment plan and techniques administered was obtained prior to commencement of treatment; (NB – in addition, written consent will be obtained for all new clients and for clients where 6months or longer has elapsed since their previous visit, on an annual basis for ongoing client management, and for dry needling, myofascial cupping and intra-oral treatment);
-
must be initialled and dated by the treating Therapist at the time of completion.
-
must clearly identify the client and the services or goods provided;
-
are to be completed & saved in MindBody & once completed, must not be deleted or edited/tampered with. If on the rare occasion that an amendment is required at a later time, MindBody will not allow a new/additional note to be created without another specific appointment being booked, so an additional note will need to be made on the original SOAP note, and the amendment clearly explained, initialled and dated by the therapist. The original SOAP note entry must not be deleted or edited and the new note must be added in the additional notes section.
-
Must detail:
-
relevant medical and health history, including allergies, previous and current medication and illness, details of previous treatment and referrals;
-
presenting conditions, including symptoms;
-
baseline measures, improvements and outcomes reached; and
-
Team members must prepare a Treatment Plan based on their professional opinion and qualifications, for each client to which they provide a treatment. The Treatment Plan must:
-
be appropriate to the particular condition with which the Client is presenting;
-
take into account:
-
the Client’s relevant medical & health/lifestyle history;
-
the Client's current condition/ presenting symptoms;
-
the Client’s future health/mobility/functional requirements; and
-
any other relevant matter following consultation with and assessment of the Client.
-
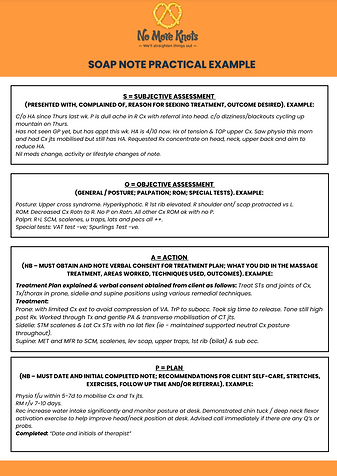
For each Treatment, the Clinical Notes must document:
-
the date of service of Treatment;
-
the provider of the service;
-
the advice and instructions given;
-
any referrals made and received;
-
details of the type of examination performed and observations made;
-
the results of diagnostic interventions or tests;
-
progression of the treatment techniques / sequence provided.
These guidelines are in keeping with the regulations provided by Medibank Private / AHM Patient Records Standards, which can be referenced here: https://www.medibank.com.au/content/dam/retail/providers/Patient%20Records%20Standards.pdf.
NB – Subject to the discretion of NMK Management, given that these terms are a contractual obligation and are a key component of all therapist’s Professional Code of Practice, NMK Management reserves the right to withhold payment of Therapist invoices &/or terminate relevant Employment or Contractor agreements if these terms are not met.